As the coronavirus pandemic continues to spread across the United States, states, payers and providers are looking for ways to expand access to telehealth. Improving access to telehealth is an essential tool in ensuring patients are able to access the healthcare services they need in as safe a manner as is possible. In order to provide our clients with quick and actionable guidance on the evolving telehealth landscape, Manatt Health has developed a comprehensive 50-state tracker for state-specific legal, policy and regulatory changes related to telehealth during the COVID-19 pandemic. Our state summaries cover state licensure flexibilities related to COVID-19, telehealth coverage and payment changes for commercial plans, and telehealth coverage and payment changes in Medicaid. This summary of findings is current as of 9:30 a.m. ET March 27, 2020.
Findings
Federal Laws, Policy and Guidance
The federal government has acted to expand access to telehealth services at a nationwide level in Medicare. In traditional, fee-for-service Medicare, CMS issued guidance that extends coverage of telehealth services to beneficiaries regardless of where they are located, allowing beneficiaries to access telehealth from their homes or from other community locations. Additionally, CMS introduced significant new flexibilities for Medicare Advantage (MA) plans to waive cost sharing for testing and treatment of COVID-19, including telehealth visits during the crisis. MA plans may also provide enrollees access to Medicare Part B services via telehealth in any geographic area and from a variety of places, including beneficiaries’ homes during this period of emergency. Lastly, HHS has granted a blanket waiver related to, among other things, out-of-state licensure, which will enable providers licensed in one state to provide services to patients in another state. This guidance does not preempt state-specific licensure restrictions, and states will need to waive these restrictions on their own. As of March 27, 45 states have introduced licensure flexibilities.
State Laws, Policy and Guidance
In Medicaid, states have broad authority to permit coverage for telehealth services. Prior to the COVID-19 emergency, many states had implemented broad coverage for telehealth, and in recent days there are even more expansive coverage policies emerging. It is critical for states to use their regulatory levers to expand upon these policies for the Medicaid populations. Medicaid programs have the broad ability to cover telehealth services and the flexibility to rapidly scale up benefits and adjust normal cost-sharing rules, making Medicaid well positioned to quickly address the needs of its beneficiaries during states of emergency. As of March 27, 42 states have taken steps to expand the use of telemedicine in their Medicaid programs during the COVID-19 emergency. Additionally, 20 states have released guidance to waive or lower telehealth copayments for their Medicaid population. During the month of March, Alaska, Minnesota, New Jersey, Vermont and West Virginia have introduced or enacted telehealth legislation to increase telehealth access and coverage. 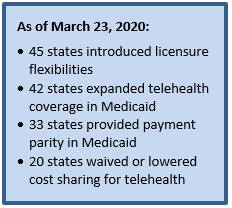
State Highlights
In Massachusetts, through executive order, Governor Charlie Baker has expanded access to telehealth services in all commercial insurers and MassHealth (state Medicaid) programs, waived all cost sharing for any medically necessary treatment delivered via telehealth related to COVID-19 at in-network providers, waived any prior authorization barriers needed to obtain medically necessary telehealth services, and established a 24-hour process to allow medical professionals to receive a license to practice in Massachusetts.
Mississippi has drastically increased its telehealth coverage during the coronavirus epidemic. The Mississippi Division of Medicaid is allowing beneficiaries to access telehealth services from home; promoting the use of personal cellular devices, computers, tablets or other web camera-enabled devices to seek and receive medical care; and waiving limitation of the use of audio-only telephonic conversations until April 30, 2020. The Mississippi State Board of Medical Licensure has waived state licensure restrictions to allow out-of-state physicians who already have a preexisting doctor-patient relationship to treat patients in Mississippi through telemedicine. Additionally, Mississippi submitted a Medicaid State Plan Amendment Telehealth Emergency Waiver to allow for telehealth service flexibilities during a state of emergency. Mississippi had payment parity for telehealth prior to the coronavirus epidemic.
New York has built on its robust telehealth policies during the coronavirus epidemic. Since Governor Andrew Cuomo announced a disaster emergency in early March, the state has waived cost sharing for in-network providers, allowed out-of-state providers and providers in New York that are not currently registered to provide telehealth services, and established telehealth reimbursement parity in Medicaid programs during the state of emergency.
Commercial Insurance
There is significant variability in commercial coverage among states. Some payers provide broad coverage for telehealth services across their network, some have contracts with third-party vendors to provide tele-visits for their members, and others don’t cover telehealth at all. Plan-specific policies about telehealth coverage and reimbursement are thus highly variable. However, states do have the ability to mandate broad coverage of telehealth services by commercial plans. As of March 23, 27 state divisions of insurance (or state equivalents) have issued bulletins to increase telehealth utility.
If you are interested in learning more about Manatt’s 50-state telehealth tracking or Insights@ManattHealth, please contact Jared Augenstein at [email protected].

